-
Team Interactieve Media 2016

-
Jaarbeeld 2016 afdeling Genetica
-
Speerpunt Cancer Center
-
Jaarbeeld Urologie 2015
-
Jaarbeeld Cardiologie 2015
-
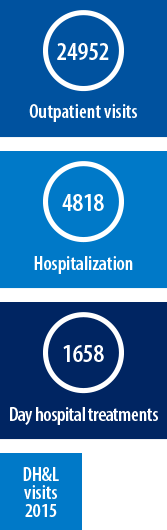
Annual Report Heart & Lungs 2015

-
Jaarbeeld Hart & Longen 2015

-
Duurzaamheidsverslag 2015, UMC Utrecht

-
Strategie facilitair bedrijf

-
Jaarbeeld Cardiologie 2014
-
Patient Centraal

-
Jaarbeeld divisie Vrouw & Baby 13/14
-
Heart & Lungs in business, annual report 2014
-
Hart & Longen in bedrijf, jaarbeeld 2014

-
Resultaten in balans
-
Jaarbeeld Cardiologie 2013

-
Annual report Cardiology 2013

-
Jaarbeeld Cardiologie 2013 A4
-
Jaarbeeld Hart & Longen 2013

-
Annual report Heart & Lungs 2013

-
MVO Magazine





'Not one patient is the same. This might be obvious, but I really only found out when I was working as an intensive care nurse and had primary responsibility for one particular patient.
This patient was a woman who had undergone a lung transplantation and who was quite a regular at the hospital. She was deteriorating, was transferred to the ICU and as her need for care increased we started getting to know each other better. What that taught me was that you need to keep the patient's background in mind. Patients are not just represented by their disorders, they each have their own background and home situation. I always find that patients like showing me pictures of their families. If you take the time to look at these, patients will be more likely later on to tell you what is wrong.
I want to see that my patients are optimally cared for and are comfortable. I also want their nonverbal communications to confirm that they feel they have been heard and that they know what I or the other healthcare professionals are doing and why.
We often use bedside computers to take patients' vital signs, which should not be viewed as an unpleasant part of the job, simply because the protocol prescribes it, but as an opportunity to make contact with patients. There is more to it than simply checking boxes on an electronic form.
I always try to have a personal talk with my patients. I observe my patients when I do so to give myself the opportunity to find out what they are thinking. This approach gives you no end of information. It might take slightly longer, but the return on investment is so great in extra knowledge, that it will allow you to help your patients better and faster in the future. And more effectively and safely.
I am also part of the division-wide Nursing Research Working Group. Whenever we want to make changes to care protocols, we first review international scientific literature. We do not introduce new intervention on a hunch but use an evidence-based approach instead. In our department, there is a white clipboard by each patient's bed. It states the name of the patient, the main treating doctor, the junior doctor, nurse and preliminary discharge date. Some people do not understand this system and wonder whether this means we want to discharge patients more quickly. But this is far from the truth.
Apart from caring for patients at the hospital, this is a reminder for us to help patients consider what they will do in the immediate future after their discharge. What about their families? Has home care been organized? We want to make the appropriate preparations for that period together with the patients. Our care continues beyond the boundaries of the hospital and does not end at the hospital doors.'

Team Interactieve Media 2016
Jaarbeeld 2016 afdeling Genetica
Speerpunt Cancer Center
Jaarbeeld Urologie 2015
Jaarbeeld Cardiologie 2015
Annual Report Heart & Lungs 2015
Jaarbeeld Hart & Longen 2015
Duurzaamheidsverslag 2015, UMC Utrecht
Strategie facilitair bedrijf
Jaarbeeld Cardiologie 2014
Patient Centraal
Jaarbeeld divisie Vrouw & Baby 13/14
Heart & Lungs in business, annual report 2014
Hart & Longen in bedrijf, jaarbeeld 2014
Resultaten in balans
Jaarbeeld Cardiologie 2013
Annual report Cardiology 2013
Jaarbeeld Cardiologie 2013 A4
Jaarbeeld Hart & Longen 2013
Annual report Heart & Lungs 2013
MVO Magazine
